Research
Studies show the effectiveness of WikiPouch® (formerly IP-Pouch),
tested & proven effective in reducing the spread of Healthcare Acquired Infections compared to Plastic Bags
CMS Mandates F880 section 483.80
Centers for Medicare & Medicaid Services
https://www.cms.gov/newsroom/fact-sheets/updated-guidance-nursing-home-resident-health-and-safety
Hospital-acquired pneumonia is killing patients.
Kaiser Health News
https://www.yahoo.com/news/hospital-acquired-pneumonia-killing-patients-080441751.html
Nonventilator hospital-acquired pneumonia: A call to action
Infection Control & Hospital Epidemiology
https://pubmed.ncbi.nlm.nih.gov/34103108/
MRSA & VRE Survived over 90 days on Plastic.
Journal of Clinical Microbiology
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC86187/
The adherence of bacteria examined was the highest on polyethylene catheters.
PubMed.gov
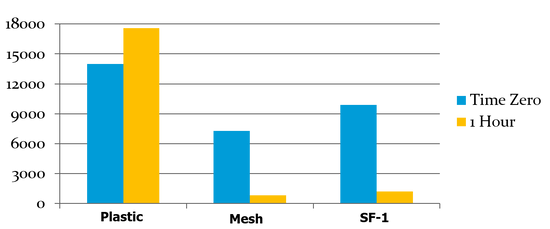
University Study: Plastic Bags vs. Mesh Bags
A recent study by Blake Brousseau, at California State University - Chico, that shows the dangers of plastic bags in healthcare. The study, under the direction of Professor Larry Hanne, Ph.D., shows that "viable bacteria were readily recovered from cannulas that had been stored in polyethylene plastic, however, numbers of recoverable bacteria decreased dramatically (84 to 99 %) following one hour storage in polypropylene mesh bags."
Healthcare Acquired Infections
Healthcare Acquired Infections U.S Statistics
Despite the steps taken to reduce Healthcare Acquired Infections or HAIs, they still remain one of the world's leading and most costly healthcare challenges. Most are preventable. All are extremely costly in human and financial terms.
The Human Cost of HAI's - Each year, nearly 2 million patients in the U.S. acquire an infection while in a healthcare setting, and nearly 100,000 die as a result. It's also estimated that 70% of HAI-causing bacteria are drug-resistant.
The Financial Cost of HAIs - Hospital stays for patients who acquire a healthcare related infection increase an average of 7-10 days, at an incremental treatment cost of over $30,000 per patient. The total annual cost to the healthcare industry totals nearly $45 billion, much of which is preventable.
Healthcare Acquired Infections Long Term Care Facility (LTCF) U.S. Statistics Estimates
More than 1.5 million residents reside in nursing homes in the United States with just under 16,000 facilities. In recent years, the acuity of illness in LTCFs has increased. LTCF residents have a risk of developing HAIs similar to that seen in acute care patients.It is estimated that there are 1.6-3.8 million Healthcare Acquired Infections which occur each year in LTCFs. The low end estimate divided by 16,000 facilities give us 100 infections per LTCF per year. The time, money and lives with this stat can be staggering. There is little HAI data & no national surveillance systems for LTCF infections.
Estimates have been calculated based on research studies and outbreak reports from the medical literature. Dolly Greene RN, CIC
Healthcare Acquired Infections On The Rise
Dame Sally Davies, the U.K.'s chief medical officer (a role equivalent to the U.S. surgeon general), warned Parliament that contagious antibiotic-resistant disease is an imminent crisis and should be included on the government's official register of possible national emergencies, right next to terrorist attacks and natural disasters, according to the Guardian.
Dr. Brad Spellberg, assistant professor of medicine at the David Geffen School of Medicine at UCLA, told LiveScience. "It's equally alarming that antibiotic drug development is at a virtual standstill, he said. "The pipeline is barren," partly because pharmaceutical companies have few incentives for developing antibiotics that people take for just a few days or weeks, Spellberg said. LiveScience.com – Fri, Jan 25, 2013
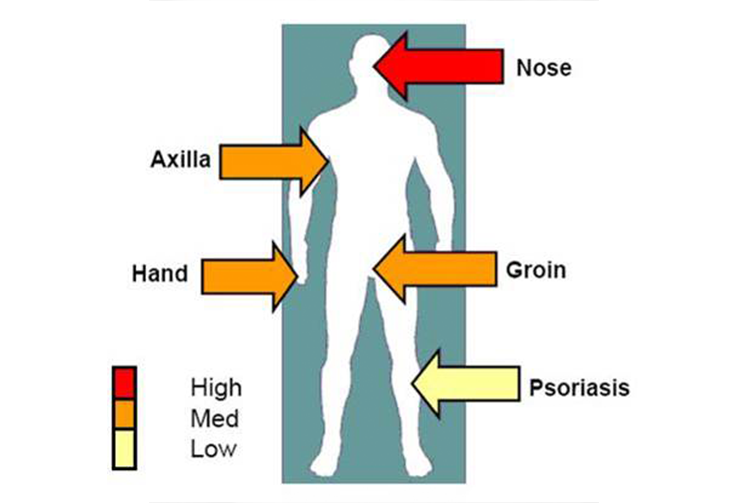
Understanding that the nose is the single greatest “hotzone” for MRSA is important in allowing infection control doctors to develop screening protocols that create the lowest drain on resources. The Nose – “Ground Zero” for MRSA colonization.
The Nose: "A Healthcare Acquired Infections Super Highway"
The nose is a high traffic area complete with north & south bound lanes. A bacterial infection in the lining of your nose can occur easily because the nasal lining that is located just inside of the nose is particularly susceptible to bacteria and subsequent infections - eHow Health.
North bound: Healthy people with normal immune systems are highly susceptible to cold virus infection once the virus enters the nose. In volunteers studies, approximately 95% of normal adults became infected when virus was dropped into the nose.
South Bound: Staph & MRSA in the nose is the most common way the bacterium is carried. Touching the nose, sneezing, wiping a runny nose, and nasal cannula use contribute to cross contamination on in health care facilities. In addition, approximately 30%-40% of all people carry Staph or MRSA in their nose. - The Nose – "Ground Zero" for MRSA colonization.
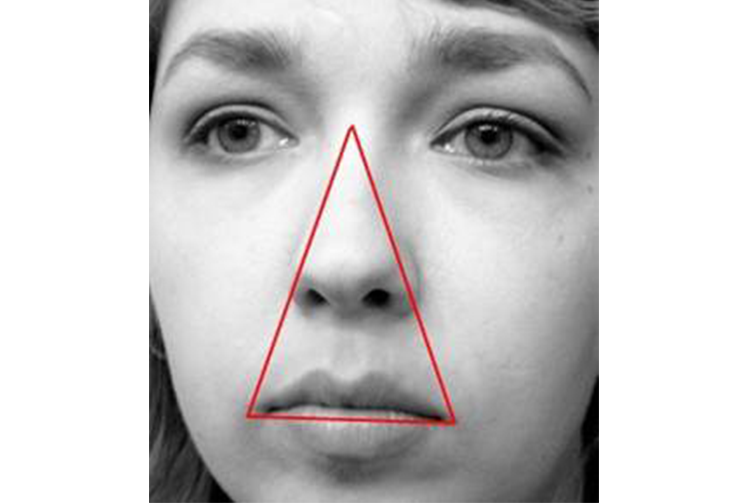
North Bound Nose
The Dr. Oz "Triangle Of Death" extends from the corners of the mouth to the bridge of the nose. The blood vessels in the triangle drain to the back of the head where it meets up with the veins at the base of the brain. From there it is a quick shot to the cavernous sinus, which receives blood from this nearby web of veins. Infections here can cause vision loss, paralysis, headaches and sometimes death.Making the nose one of the most vulnerable body parts in the fight against Healthcare Acquired Infections.
South Bound Lane
Staph and MRSA bacteria like warm, moist environments and commonly live in the nose. Staph Infections resourcesUp to 40% of the population have staph in their nose either persistently or intermittently. Most of the time they do not suffer any illness as a result, even though some of these staph are MRSA. ABC NewsIt was previously accepted that only 1% of population carry MRSA in their nose, however, new reports say that number is now 5%.
MRSA Is On The Rise
Some studies have found that as many as 23% to 35% of residents in Veterans’ Affairs long-term care facilities become colonized with MRSA – that is, carry the bacteria in their noses – over one to two years. In freestanding nursing homes, studies indicate that 9 to 12% of residents are colonized. Chicago Tribune (2008)
MRSA infections are occurring with rising frequency in hospitals, where staph bacteria wreak havoc on patients who are already weakened. Hospital-acquired infections are blamed for more than 100,000 deaths in the U.S. each year. 63% of staph infections were caused by MRSA in 2004, in contrast with only 22% in 1995 and 2% in 1974. - PBS
Every time these older people touch their nose and then reach for a phone or a bed rail which a nursing aid then touches, there's an opportunity to transmit the bacterium. In hospitals, it's understood that patients colonized with MRSA should be isolated and strict precautions taken. In nursing homes, isolation generally doesn't occur. Chicago Tribune (2008)
MRSA & VRE Survival On Materials
The purpose of this study was to determine the survival of 22 gram-positive bacteria (vancomycin-sensitive and -resistant enterococci and methicillin-sensitive and -resistant staphylococci) on five common hospital materials: smooth 100% cotton (clothing), 100% cotton terry (towels), 60% cotton–40% polyester blend (scrub suits and lab coats), 100% polyester (privacy drapes), and 100% Polyethylene plastic (splash aprons).
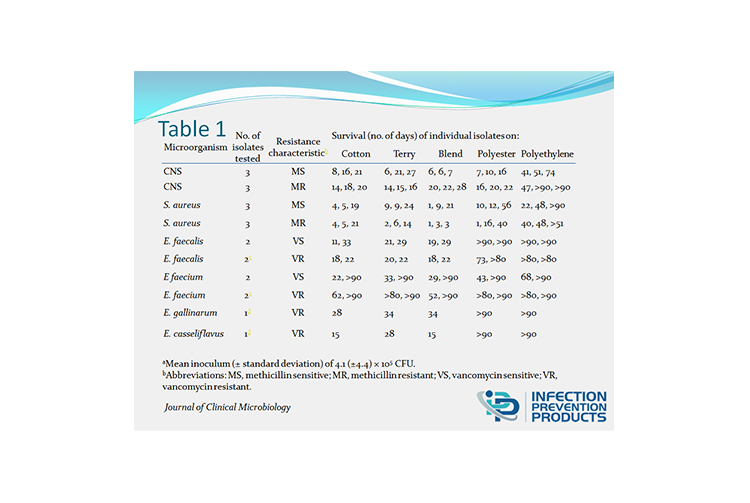
The long survival of these bacteria, including MRSA and VRE, on commonly used hospital fabrics, such as scrub suits, lab coats, and hospital privacy drapes, underscores the need for meticulous contact control procedures and careful disinfection to limit the spread of these bacteria.All staphylococci tested survived for at least 1 day on all fabrics and plastic (Table 1). Staphylococcal viability was longest on polyester (1 to 56 days) and on polyethylene plastic (22 to >90 days). There was a tendency for the size of the microbial inoculum to increase the survival time of the CNS tested; however, even a few hundred bacteria survived for days on most fabrics.
MRSA & VRE Survival Study Conclusion
In conclusion, data in this study indicate that staphylococci and enterococci can survive for extended periods of time on materials commonly worn by patients and health care workers and on various other fabrics in the hospital environment.Hence, the lengthy survival of these microorganisms on these various materials underscores the importance of both meticulous contact control procedures and thorough disinfection of hospital fabrics and plastic to minimize the spread of gram-positive microorganisms such as MRSA and VRE. -Journal of Clinical Microbiology
Bacteria in Reused Plastic Water Bottles
In 2003 the University of Calgary conducted a study of 75 plastic water bottles from an elementary school classroom. The bacteria levels were so high in the bottles that, had the water been from the tap, a boil-water order would have been issued. However, the study concluded that the high bacteria levels were more associated with poor hygiene practices than with the plastic bottles themselves. Bacteria grow naturally in moist, warm environments, and virtually any container can provide the right circumstances for bacterial growth… Such as a "Plastic Bag".
So What Do We Know About Healthcare Acquired Infections?
Healthcare Acquired Infections or HAI’s are on the rise & the nose is a HAI Super Highway! Bacteria grows in warm pockets with little or no airflow… Plastic bags are a perfect place to grow Bacteria. VRE & MRSA survive on Plastic longer than on any other Material… (Journal of Clinical Microbiology) & YET we are storing nasal cannulas in a Plastic Bag.
California State University Study
In a study at a California State University completed February 27, 2013, the time zero numbers were captured to chart the actual increase or decrease of the staph microbial counts on the nasal cannula in a Plastic Bag, Polyester Mesh Bag & Spun Fiber Polypropylene Bag (SF-1) for 1 hour.
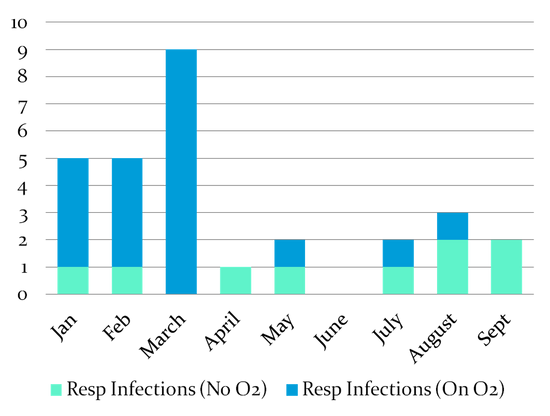
WikiPouch® (formerly IP-Pouch) Field Trials & Testimonials
At Country Villa Riverview in Susanville CA, the WikiPouch® (formerly IP-Pouch) was tested over a 6 month period starting in April 2012 and demonstrated more than a 75% reduction in URIs. The reduction was so great that the Director of Nurses Steve Tank was quoted saying: "The WikiPouch® (formerly IP-Pouch) from Infection Prevention Products is an amazing product. It has reduced respiratory infections immensely. I don't know how we've lasted this long without it”.
-
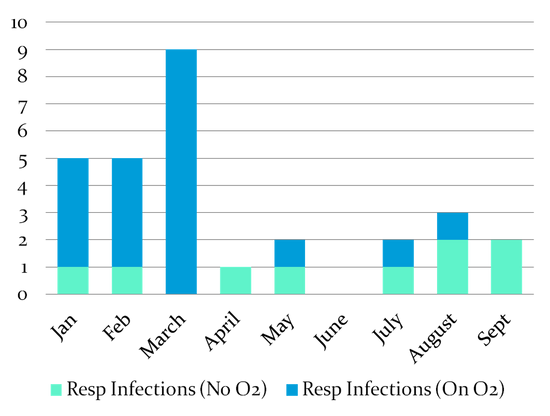
During a Study at Windsor Chico Care center, in reviewing the Healthcare Acquired Infections URIs within the facility, there was a decrease in URIs in Nov & Dec 2012 from storing the nasal cannulas in the WikiPouch® (formerly IP-Pouch) compared to Nov & Dec 2011 during which time the nasal cannula were stored in plastic bags. The decrease in URIs was 63% & 50% respectively.We attribute the decrease to the following factors: Increased staff awareness and adherence of the facility P & P regarding URIs and the use of the WikiPouch® (formerly IP-Pouch) product which allowed for more complete drying of the equipment and thus the decreased potential of URIs. Barbara Santos, DSD, Windsor Chico Care Center Barbara further went on to say: "Thank you for this product. It has been a long time coming. It is so easy, Sticks to w/c, bedside stands or nebulizers. Has helped reduced Healthcare Acquired Infections and will surely help reduce readmissions to the acute setting."
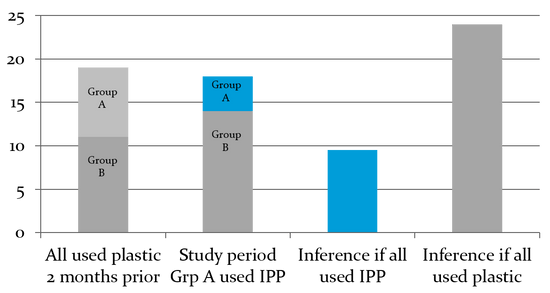
IPP Control Group Study
In a two month control group study at SANDPIPER Premier Senior Living "SNF" under the direction of Eric Hadley, Executive Director & MHA, FACHE, FACHCA, the study parameters compared the URIs in residents that continued storing their nasal cannula in a plastic bag (Group B) vs. those residents (roughly half) who, during the study, stored their nasal cannula in the WikiPouch® (formerly IP-Pouch) (Group A). Study period, Jan 23 to March 25, 2013. Group B increased 27%
Plastic Bags Cost Too Much!
PLASTIC BAGS Need to be Replaced Each Week: Plastic bags, plus the time to put them up each week, cost over $5 per month. The WikiPouch® (formerly IP-Pouch) is replaced once per month with an MSRP of only $1.99. (volume discounts available)
PLASTIC BAGS Allow Microbes to Survive and Thrive:MRSA & VRE survived longer on Plastic (Over 90 Days) than on any material tested that is common in healthcare facilities. - Journal of Clinical Microbiology. In University studies, Plastic Bags increased Staph microbes 28% in 1 hour on a nasal cannula.
PLASTIC BAGS Increase Respiratory Infections: In field trials, Plastic Bags increased respiratory infection while the WikiPouch® (formerly IP-Pouch) reduced respiratory infections over 60% compared to the use of Plastic Bags.
PLASTIC BAGS Increase Mortality: In nursing homes, respiratory infections caused by influenza, parainfluenza, and respiratory syncytial viruses are often fatal. Nursing homes, which generally have older and frailer residents, can experience attack rates up to 60% and case fatality rates as high as 55%. -Infectious Disease Clinics of North America 2007
Conclusion
Healthcare Acquired Infections HAI are getting worse & so are the costs, both human and financial. The nose is a HAI super-highway. It is a high traffic area complete with north and south bound lanes that must be monitored. Understanding the survival rate and the adherence of microbes to common healthcare materials underscores the need for meticulous contact control procedures and careful disinfection to limit the spread of these bacteria. URIs and other Healthcare Acquired Infections cost each LTCF, even if insurance covers all of the reimbursements. Estimates are over $5,000 per infection. Deploying the WikiPouch® (formerly IP-Pouch) in your facility has shown to be a proven method to reduce the spread of many Healthcare Acquired Infections which will help save time, money & lives.